The COVID-19 pandemic has left an indelible mark on global health, affecting millions of individuals across the world. While the primary focus has been on the respiratory implications of the virus, emerging evidence suggests that COVID-19 can also have significant cardiovascular effects.
Understanding these post-COVID cardiovascular complications is crucial for improving patient outcomes and managing long-term health risks. COVID-19, caused by the SARS-CoV-2 virus, primarily targets the respiratory system, leading to symptoms such as fever, cough, and shortness of breath. However, the virus’s impact extends beyond the lungs, affecting multiple organ systems, including the heart.
Recent studies have shown that individuals recovering from COVID-19 may experience a range of heart-related issues, from mild symptoms to severe conditions like heart failure and myocarditis. The cardiovascular complications associated with COVID-19 are not limited to those with pre-existing heart conditions. Even healthy individuals can experience heart damage due to the virus. This damage can manifest in various forms, including inflammation of the heart muscle (myocarditis), blood clots, and arrhythmias. These complications can arise during the acute phase of the infection or as part of the long-term effects, often referred to as “Long COVID.” Recognizing the importance of these findings, healthcare providers are now paying closer attention to the cardiovascular health of COVID-19 survivors. Early detection and management of heart-related issues are essential for preventing further complications and ensuring better health outcomes.
For those experiencing symptoms such as chest pain, palpitations, or shortness of breath after recovering from COVID-19, seeking medical advice is imperative. Understanding the potential risks and taking proactive measures can significantly improve the quality of life for those affected by the virus.
Acute Cardiac Injury
Mechanisms
COVID-19 has been shown to cause acute cardiac injury through several mechanisms. One of the primary ways is the direct viral invasion of heart tissues. The SARS-CoV-2 virus binds to the ACE2 receptors, which are abundantly present in the heart. This binding facilitates the entry of the virus into cardiac cells, leading to direct damage and inflammation. This direct invasion can result in myocarditis, a condition characterized by inflammation of the heart muscle, which can severely impair cardiac function. Another significant mechanism is the inflammatory cytokine storm. COVID-19 triggers an exaggerated immune response, releasing a large number of cytokines into the bloodstream. This cytokine storm can cause widespread inflammation, including in the heart. The excessive inflammatory response can lead to damage of the heart tissues, contributing to conditions such as myocarditis and pericarditis. The inflammation can also exacerbate pre-existing cardiovascular conditions, leading to more severe outcomes. Additionally, COVID-19 can cause an oxygen supply-demand imbalance. The virus can lead to severe respiratory distress, reducing the oxygen levels in the blood. The heart, which requires a constant supply of oxygen to function effectively, can suffer from this reduced oxygen availability. This imbalance can lead to myocardial ischemia, where the heart muscle is deprived of adequate oxygen, potentially resulting in myocardial infarction (heart attack).
Clinical Manifestations
The clinical manifestations of acute cardiac injury in COVID-19 patients are varied and can range from mild to severe. One of the key indicators of cardiac injury is elevated cardiac biomarkers. Blood tests often reveal increased levels of troponin, a protein released when the heart muscle is damaged. Elevated troponin levels are a strong indicator of myocardial injury and are commonly observed in COVID-19 patients with severe disease. Symptoms such as chest pain and shortness of breath are also common in patients experiencing acute cardiac injury. These symptoms can be indicative of underlying conditions such as myocarditis or myocardial infarction. Chest pain, in particular, can be a sign of myocardial ischemia, where the heart muscle is not receiving enough oxygen. Shortness of breath can result from both respiratory and cardiac complications, making it a critical symptom to monitor in COVID-19 patients. There is also an increased incidence of myocardial infarction among COVID-19 patients. The virus can cause plaque rupture in the coronary arteries, leading to the formation of blood clots. These clots can obstruct blood flow to the heart, resulting in a heart attack. The inflammatory response triggered by the virus can also contribute to the instability of atherosclerotic plaques, increasing the risk of myocardial infarction.
Treatment Approaches
Treating acute cardiac injury in COVID-19 patients requires a multifaceted approach. One of the primary treatment strategies is antiviral therapy. Medications that target the SARS-CoV-2 virus can help reduce the viral load in the body, potentially mitigating the direct damage to the heart tissues. Antiviral drugs such as remdesivir have been used to treat COVID-19 and may have a role in preventing or reducing cardiac injury. Anti-inflammatory medications are also crucial in managing acute cardiac injury. Given the role of the inflammatory cytokine storm in causing heart damage, drugs that reduce inflammation can be beneficial. Corticosteroids like dexamethasone have been shown to reduce mortality in severe COVID-19 cases by dampening the inflammatory response. Other anti-inflammatory agents, such as interleukin-6 inhibitors, are also being explored for their potential benefits in reducing cardiac inflammation. Supportive care and cardiac monitoring are essential components of the treatment plan. Patients with acute cardiac injury require close monitoring of their cardiac function, including regular electrocardiograms (ECGs) and echocardiograms. Supportive care measures, such as oxygen therapy and mechanical ventilation, may be necessary for patients with severe respiratory distress. In cases of myocardial infarction, standard treatments such as antiplatelet therapy, anticoagulation, and revascularization procedures may be required. Understanding the mechanisms, clinical manifestations, and treatment approaches for acute cardiac injury in COVID-19 patients is crucial for improving patient outcomes. Early recognition and prompt management of these complications can significantly reduce the risk of long-term COVID heart issues and improve the overall prognosis for affected individuals.
Long-term Cardiovascular Effects
Myocarditis and Cardiomyopathy
One of the most concerning long-term cardiovascular effects of COVID-19 is myocarditis, which is the chronic inflammation of the heart muscle. COVID myocarditis can persist long after the initial infection has resolved, leading to ongoing symptoms and complications. The inflammation can cause the heart muscle to become swollen and weakened, impairing its ability to pump blood effectively. This condition can be particularly debilitating, as it may lead to chronic fatigue, chest pain, and shortness of breath. The potential for heart muscle weakening is a significant concern. When the heart muscle is inflamed and damaged, it can lose its strength and elasticity. This weakening can progress to cardiomyopathy, a condition where the heart muscle becomes enlarged, thickened, or rigid. Cardiomyopathy can severely impact the heart’s ability to function, leading to symptoms such as fluid retention, swelling in the legs, and difficulty breathing. In severe cases, it can result in heart failure, where the heart is unable to pump enough blood to meet the body’s needs. The risk of heart failure is a critical aspect of post-COVID heart health. Heart failure can develop gradually as the heart muscle continues to weaken over time. Patients with COVID-19 heart damage are at an increased risk of developing heart failure, especially if they have pre-existing cardiovascular conditions. Managing this risk requires ongoing medical supervision, lifestyle modifications, and potentially, the use of medications to support heart function and reduce symptoms.
Arrhythmias
Arrhythmias, or irregular heartbeats, are another long-term cardiovascular effect observed in COVID-19 survivors. These irregular heartbeats can occur as a result of the virus’s impact on the electrical pathways of the heart. COVID-induced heart conditions can disrupt the normal rhythm of the heart, leading to arrhythmias that can be both symptomatic and asymptomatic. Patients may experience palpitations, dizziness, or even fainting spells as a result of these irregular heartbeats. The need for continuous monitoring of arrhythmias is paramount. Patients who have recovered from COVID-19 but continue to experience symptoms such as palpitations or dizziness should undergo regular cardiac evaluations. Continuous monitoring can help detect arrhythmias early and allow for timely intervention. Holter monitors, which record the heart’s activity over 24 to 48 hours, and event monitors, which record heart activity over longer periods, can be useful tools in diagnosing and managing arrhythmias. Potential treatments for arrhythmias include medication and ablation. Medications such as beta-blockers, calcium channel blockers, and antiarrhythmic drugs can help control the heart rate and rhythm. In cases where medication is not effective, catheter ablation may be considered. This procedure involves threading a catheter through the blood vessels to the heart, where it uses heat or cold energy to destroy the areas of heart tissue causing the arrhythmia. Ablation can be an effective treatment for certain types of arrhythmias, providing long-term relief for patients.
Thromboembolic Events
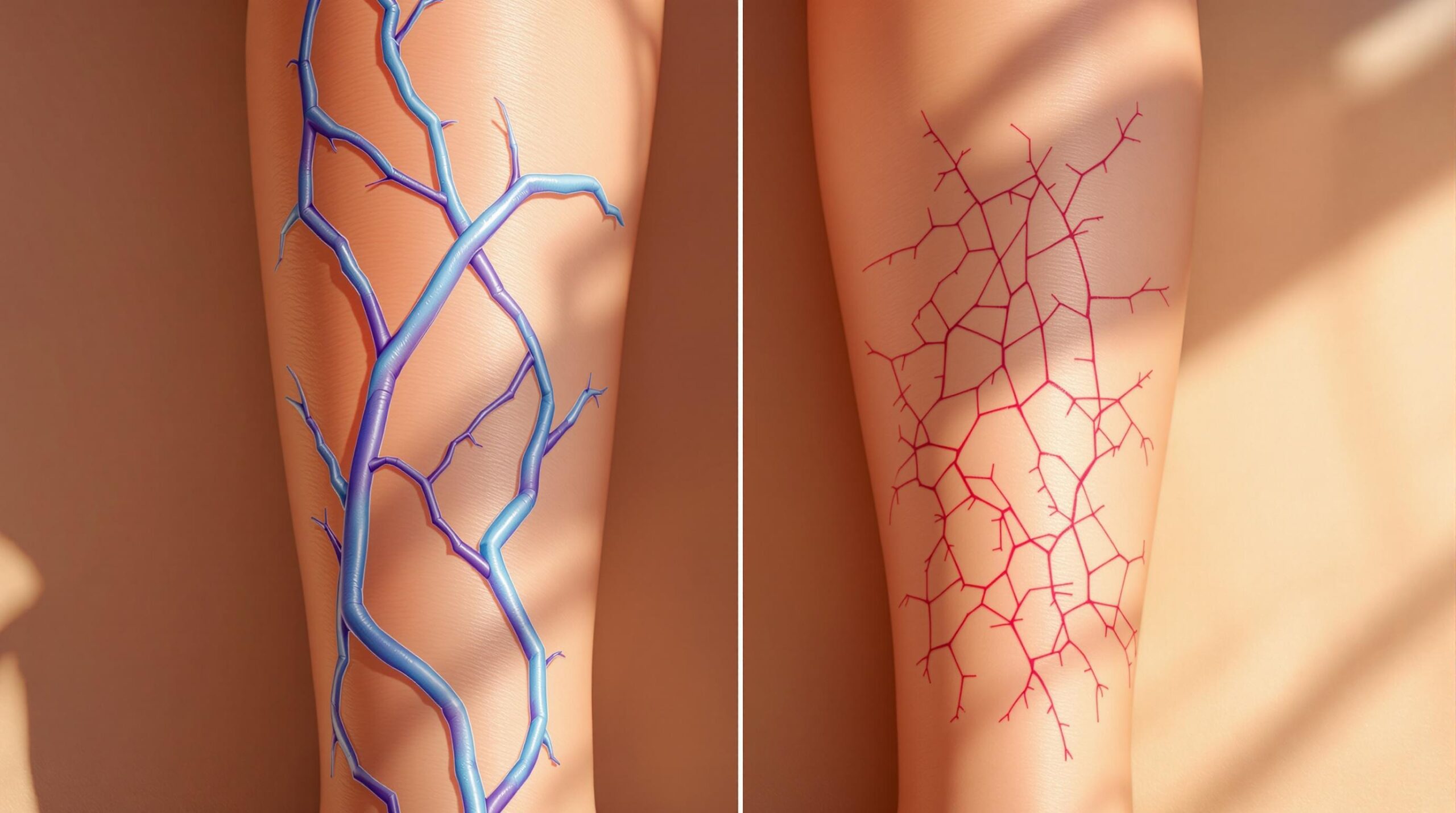
Thromboembolic events, including the formation of blood clots, are a significant long-term cardiovascular complication of COVID-19. The virus can increase the risk of blood clot formation, leading to conditions such as deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT occurs when a blood clot forms in a deep vein, usually in the legs, while PE occurs when a clot breaks free and travels to the lungs, causing a blockage. These conditions can be life-threatening and require immediate medical attention. The association between COVID-19 and thromboembolic events is well-documented. The inflammatory response triggered by the virus can lead to a hypercoagulable state, where the blood is more prone to clotting. This increased risk of blood clots can persist long after the acute phase of the infection, making it essential for patients to be aware of the signs and symptoms of DVT and PE. Symptoms of DVT include swelling, pain, and redness in the affected leg, while symptoms of PE include sudden shortness of breath, chest pain, and coughing up blood. The importance of anticoagulant therapy in managing thromboembolic events cannot be overstated. Anticoagulants, or blood thinners, can help prevent the formation of new clots and reduce the risk of existing clots growing larger. Patients recovering from COVID-19 who are at high risk for thromboembolic events may be prescribed anticoagulant therapy as a preventive measure. Regular monitoring and follow-up with healthcare providers are essential to ensure the effectiveness and safety of anticoagulant therapy. Understanding the long-term cardiovascular effects of COVID-19 is crucial for managing the health of survivors. Myocarditis, cardiomyopathy, arrhythmias, and thromboembolic events are significant concerns that require ongoing medical attention and intervention. By recognizing these potential complications and implementing appropriate treatment strategies, healthcare providers can help improve the long-term outcomes for individuals affected by COVID-19.
Strategies for Mitigation and Management
Early Detection and Screening
Early detection and screening are pivotal in managing the cardiovascular effects of COVID-19. Regular cardiac assessments can help identify COVID-19 heart damage before it progresses to more severe conditions. These assessments should be a routine part of follow-up care for individuals who have recovered from COVID-19, especially those who experienced severe symptoms or required hospitalization. Regular monitoring can help detect early signs of heart issues after COVID, allowing for timely intervention and treatment. The use of imaging techniques and biomarkers is essential in the early detection of post-COVID heart disease. Echocardiograms, cardiac MRI, and CT scans can provide detailed images of the heart, helping to identify structural abnormalities, inflammation, and other signs of damage. Biomarkers such as troponin, B-type natriuretic peptide (BNP), and C-reactive protein (CRP) can indicate myocardial injury, heart failure, and inflammation, respectively. These diagnostic tools are invaluable in assessing the cardiovascular health of COVID-19 survivors. Identifying high-risk patients is another critical aspect of early detection. Individuals with pre-existing cardiovascular conditions, diabetes, hypertension, and obesity are at a higher risk of developing COVID-19 cardiac complications. Additionally, those who experienced severe COVID-19 symptoms or required intensive care are more likely to suffer from long-term COVID heart issues. By identifying these high-risk patients, healthcare providers can prioritize them for regular cardiac assessments and implement preventive measures to mitigate the risk of severe complications.
Lifestyle Modifications
Lifestyle modifications play a crucial role in managing post-COVID heart health. Adopting a heart-healthy diet and engaging in regular physical activity can significantly improve cardiovascular outcomes. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help reduce inflammation and support overall heart health. Limiting the intake of processed foods, sugary beverages, and excessive salt can also help manage blood pressure and reduce the risk of cardiovascular disease. Exercise is another vital component of maintaining post-COVID heart health. Regular physical activity can improve cardiovascular fitness, reduce inflammation, and enhance overall well-being. Patients recovering from COVID-19 should aim for at least 150 minutes of moderate-intensity aerobic exercise per week, along with muscle-strengthening activities on two or more days per week. However, it is essential to consult with a healthcare provider before starting any new exercise regimen, especially for those with COVID-induced heart conditions. Smoking cessation is critical for improving cardiovascular health. Smoking is a significant risk factor for heart disease, and quitting can have immediate and long-term benefits. Healthcare providers should offer resources and support to help patients quit smoking, including counseling, nicotine replacement therapy, and medications. Reducing or eliminating tobacco use can significantly lower the risk of COVID-19 and heart failure, as well as other cardiovascular complications. Stress management techniques are also essential for maintaining post-COVID heart health. Chronic stress can negatively impact cardiovascular health by increasing blood pressure, heart rate, and inflammation. Techniques such as mindfulness meditation, deep breathing exercises, yoga, and regular physical activity can help manage stress levels. Additionally, seeking support from mental health professionals, support groups, and loved ones can provide emotional relief and improve overall well-being.
Ongoing Research and Clinical Trials
Ongoing research and clinical trials are crucial for advancing our understanding of post-COVID cardiovascular health and developing effective treatments. Current studies are exploring the long-term cardiovascular effects of COVID-19, including the mechanisms behind COVID heart inflammation, myocarditis, and other complications. These studies aim to identify risk factors, improve diagnostic methods, and develop targeted therapies to manage and mitigate the cardiovascular effects of COVID-19. Exploration of novel treatments and interventions is a key focus of ongoing research. Researchers are investigating various therapeutic approaches, including antiviral drugs, anti-inflammatory medications, and immunomodulatory therapies, to address COVID-19 cardiac complications. Additionally, studies are examining the potential benefits of existing cardiovascular medications, such as ACE inhibitors, beta-blockers, and anticoagulants, in managing post-COVID heart disease. These efforts aim to provide evidence-based guidelines for the treatment and management of COVID-related heart problems. Opportunities for patient participation in research are essential for advancing our understanding of post-COVID cardiovascular health. Clinical trials and observational studies rely on the participation of individuals who have recovered from COVID-19 to gather valuable data and insights. Patients can contribute to research efforts by enrolling in clinical trials, providing blood samples, and participating in follow-up assessments. By participating in research, patients can help accelerate the development of effective treatments and improve outcomes for others affected by COVID-19 and cardiovascular health issues. In conclusion, early detection and screening, lifestyle modifications, and ongoing research are critical strategies for mitigating and managing the long-term cardiovascular effects of COVID-19. By implementing these strategies, healthcare providers can improve the quality of life for COVID-19 survivors and reduce the burden of cardiovascular complications. Understanding and addressing the cardiovascular effects of COVID-19 is essential for ensuring better health outcomes and enhancing the overall well-being of affected individuals.
Conclusion
The COVID-19 pandemic has brought to light a myriad of health challenges, with cardiovascular complications emerging as a significant concern. The virus’s impact on the heart is multifaceted, involving acute cardiac injury, long-term cardiovascular effects, and an increased risk of thromboembolic events. Acute cardiac injury can result from direct viral invasion of heart tissues, inflammatory cytokine storms, and oxygen supply-demand imbalances, leading to conditions such as myocarditis, myocardial infarction, and heart failure. Long-term effects include chronic myocarditis, cardiomyopathy, arrhythmias, and thromboembolic events, all of which can severely impact post-COVID heart health. Understanding these complications is crucial for healthcare providers and patients alike. Awareness of the potential for COVID-19 heart damage can lead to more vigilant monitoring and early detection of cardiovascular issues. Regular cardiac assessments, the use of imaging techniques, and the identification of high-risk patients are essential steps in mitigating the impact of these complications. Recognizing symptoms such as chest pain, shortness of breath, palpitations, and swelling can prompt timely medical intervention, potentially preventing more severe outcomes. The importance of awareness, early detection, and continuous research cannot be overstated.
Early detection through regular screening and the use of biomarkers can help identify cardiovascular issues before they become severe. Lifestyle modifications, including a heart-healthy diet, regular exercise, smoking cessation, and stress management, play a vital role in maintaining cardiovascular health and preventing further complications. These proactive measures can significantly improve the quality of life for COVID-19 survivors and reduce the burden of long-term COVID heart issues. Continuous research and clinical trials are essential for advancing our understanding of post-COVID cardiovascular health and developing effective treatments. Ongoing studies are exploring the mechanisms behind COVID-19 cardiac complications, the potential benefits of existing medications, and novel therapeutic approaches. Patient participation in research efforts is crucial for gathering valuable data and accelerating the development of evidence-based guidelines for managing COVID-related heart problems. In conclusion, the cardiovascular effects of COVID-19 present a significant challenge that requires a comprehensive approach to management and treatment. By raising awareness, prioritizing early detection, and supporting continuous research, we can improve outcomes for individuals affected by COVID-19 and cardiovascular health issues. Understanding and addressing these complications is essential for ensuring better health outcomes and enhancing the overall well-being of those impacted by the virus.