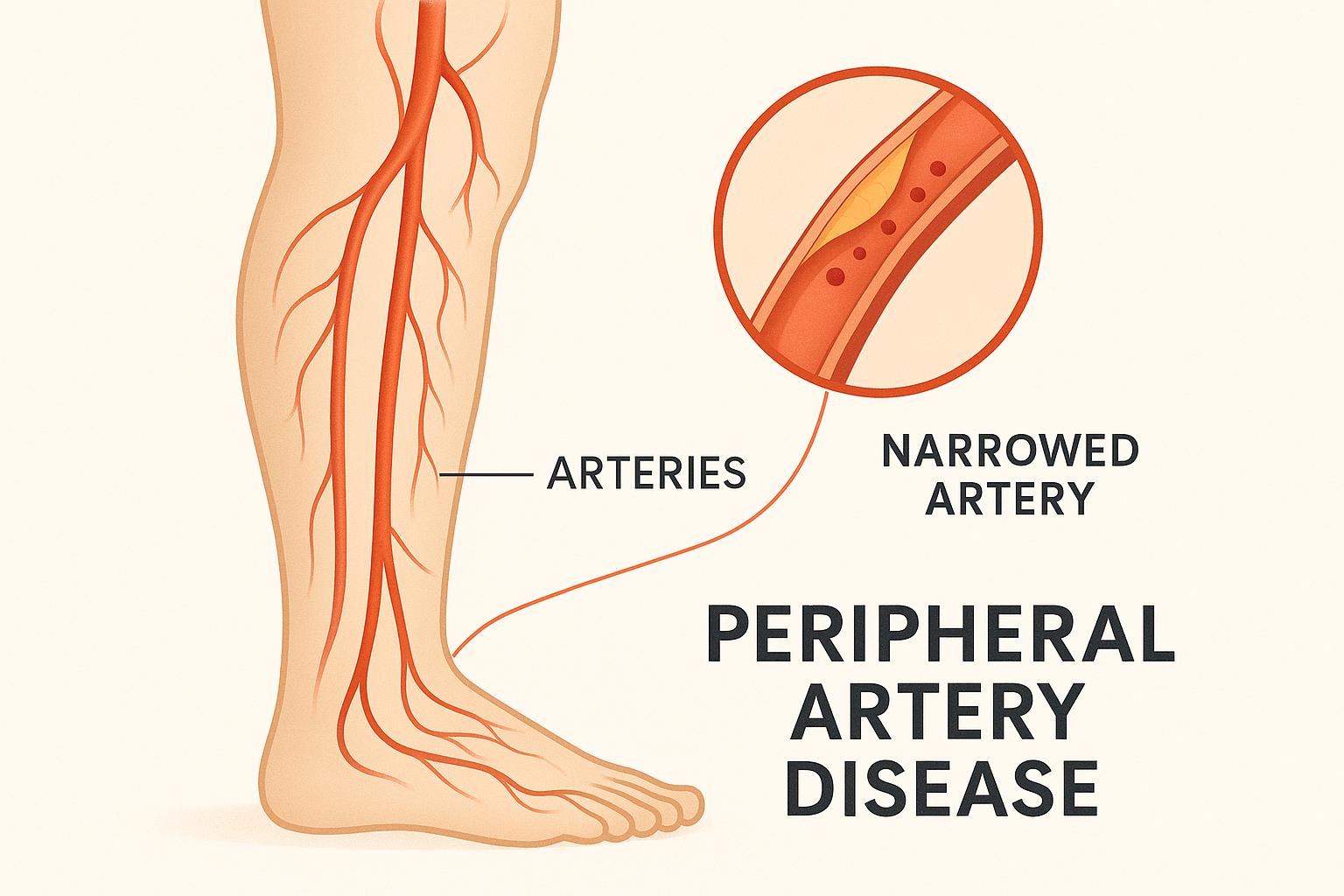
Peripheral Artery Disease (PAD) is a condition where narrowed arteries reduce blood flow, primarily to the legs and feet. This affects over 8 million Americans aged 40 and older. PAD often stems from atherosclerosis – plaque buildup in arteries – and can lead to serious complications like stroke, gangrene, or even amputation if left untreated.
Key Takeaways:
- Symptoms: Leg pain during activity (intermittent claudication), slow-healing sores, numbness, or cold feet. Not all cases show symptoms.
- Risk Factors: Age (60+), smoking, high blood pressure, diabetes, high cholesterol.
- Prevention: Regular exercise, quitting smoking, healthy diet, and managing conditions like diabetes or high blood pressure.
- Treatment Options: Lifestyle changes, medications (e.g., antiplatelets, statins), and in severe cases, procedures like angioplasty or bypass surgery.
PAD often goes unnoticed, so early detection and management are essential to prevent serious outcomes. Regular screenings, especially for high-risk groups, can make a significant difference.
Common PAD Symptoms
Main Warning Signs
Peripheral Artery Disease (PAD) often comes with clear physical signs. One of the most common is intermittent claudication – leg pain that shows up during physical activity and eases with rest.
Other noticeable changes in the affected limb might include pale, discolored, or bluish skin, along with reduced hair and toenail growth. You might also notice one foot feeling colder than the other, or sores and wounds on the toes, feet, or legs that heal very slowly – or not at all.
"Without treatment, PAD may cause sores, infections, and even the loss of a limb." – NHLBI, NIH
It’s worth mentioning that PAD-related leg pain is different from arthritis. Arthritis pain usually centers on the joints, while PAD pain affects the muscles and tends to improve with rest. However, some symptoms can be less obvious, as detailed below.
Hidden Symptoms
PAD doesn’t always present with clear warning signs. In fact, more than half of individuals with PAD experience subtle or non-typical symptoms, and about 20% report no symptoms at all. Some of the less obvious signs include:
- Tingling or numbness in the legs or feet
- Weakness in the legs that affects walking
- Pain at rest in more severe cases
- Erectile dysfunction, which can signal reduced blood flow
For people with diabetes, PAD symptoms can sometimes be confused with diabetic neuropathy, as both conditions may cause burning or painful sensations in the feet or thighs.
| Typical Symptoms | Hidden Symptoms |
|---|---|
| Leg cramping during activity | Tingling or numbness in legs/feet |
| Noticeable skin color changes | Weakness affecting walking stability |
| One foot colder than the other | Subtle balance issues |
| Wounds that heal very slowly | Mild discomfort at rest |
Peripheral Arterial Disease (PAD) – Comprehensive …
Risk Factors
Understanding what contributes to PAD helps us identify symptoms early and take timely action.
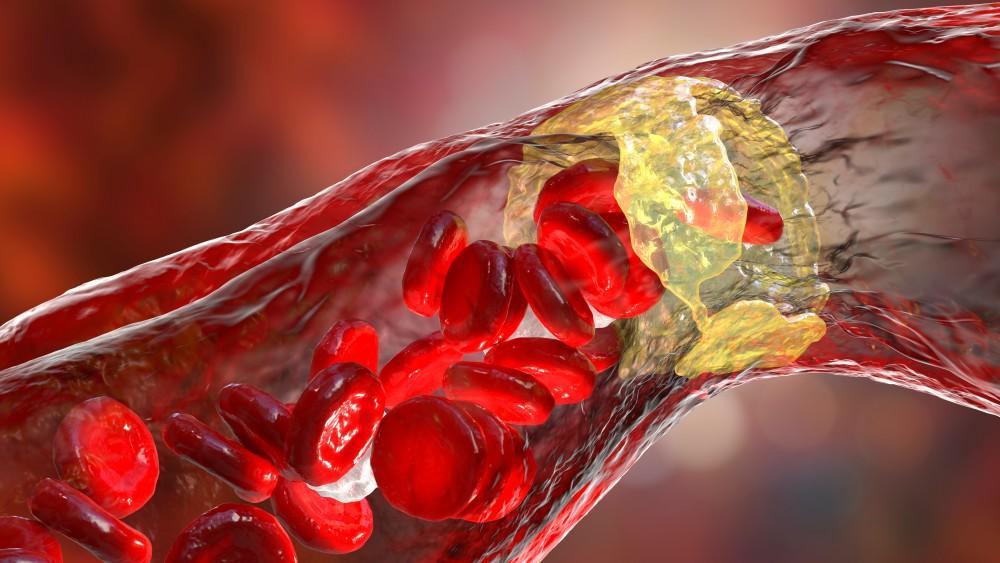
How Plaque Build-Up Impacts the Body
Peripheral Artery Disease (PAD) primarily stems from a condition called atherosclerosis. This happens when plaque – a mix of fat, cholesterol, fibrous tissue, and calcium – builds up inside arteries. Over time, this accumulation narrows the arteries, restricting blood flow to the limbs and organs. Reduced oxygen-rich blood flow often results in pain and cramping during physical activity.
Common Risk Factors
Being aware of the factors that increase your risk of PAD is critical for early prevention:
| Risk Factor Type | Examples | Impact |
|---|---|---|
| Age-Related | 65 years or older | Most PAD cases in the U.S. occur in this group |
| Medical Conditions | Diabetes, High Blood Pressure | Strongly linked to higher PAD risk |
| Lifestyle Choices | Smoking, Sedentary Behavior | Directly harms arterial health |
| Genetic Factors | Family History | Greater likelihood if relatives had PAD |
Globally, PAD affects around 200 million people, including up to 45 million Americans. Certain groups, such as African Americans, face a higher risk compared to others.
Smoking plays a major role in increasing PAD risk. It constricts blood vessels, reduces blood flow to the legs, and damages vessel walls. It also worsens cholesterol levels, creating conditions that encourage PAD.
Work environments that involve long periods of sitting or exposure to pollutants may also contribute to an elevated risk.
sbb-itb-4bfbcfd
Treatment Methods
Peripheral Artery Disease (PAD) management involves a mix of lifestyle changes, medications, and surgical procedures.
Daily Habits That Help
Making key lifestyle adjustments can ease PAD symptoms and slow its progression. Quitting smoking is a top priority, as it significantly reduces symptoms and lowers the risk of complications.
Regular exercise is another powerful tool. A structured program often includes:
| Exercise Component | Frequency | Duration | Benefits |
|---|---|---|---|
| Treadmill Walking | 3–4 times per week | 30–45 minutes | Boosts blood flow |
| Leg Strengthening | 2–3 times per week | 20–30 minutes | Enhances endurance |
| Flexibility Exercises | Daily | 10–15 minutes | Reduces stiffness |
Diet also plays a role. The Mediterranean diet – packed with fruits, vegetables, whole grains, and healthy fats – has been linked to better management of PAD symptoms. Additionally, checking your feet daily can help catch and prevent complications early.
These lifestyle changes work alongside medical treatments to improve overall outcomes for PAD patients.
Medical Options
Medications are often prescribed to manage symptoms and prevent complications. Common types include:
| Medication Type | Purpose | Examples |
|---|---|---|
| Antiplatelet Agents | Prevent blood clots | Aspirin, Clopidogrel |
| Statins | Lower cholesterol | Multiple brands available |
| Cilostazol | Increases walking distance | Prescription required |
"In most cases, lifestyle changes, exercise and claudication medications are enough to slow the progression or even reverse the symptoms of PAD." – American Heart Association
Your doctor will recommend the right combination of treatments based on your medical history and unique needs.
Surgical Procedures
If medications and lifestyle changes aren’t enough, surgical options may be necessary. These include:
-
Angioplasty and Stenting
A minimally invasive procedure where a small balloon is used to open blocked arteries. A stent is often placed afterward to keep the artery open. -
Bypass Surgery
For severe blockages, this procedure creates a new pathway for blood to flow around the obstructed artery.
These approaches are typically reserved for more advanced cases of PAD.
Prevention and New Treatments
Ways to Prevent PAD
To reduce the risk of PAD, focus on managing key factors through regular check-ups and adopting heart-friendly habits.
Health screenings are especially important for people over 60 or those with risk factors. PAD often goes unnoticed until an artery is more than 50% narrowed.
| Prevention Strategy | Recommended Actions | Benefits |
|---|---|---|
| Physical Activity | 150 minutes of moderate or 75 minutes of vigorous exercise weekly | Boosts circulation and overall heart health |
| Diet Modifications | Prioritize heart-healthy foods; limit sodium and added sugars | Helps regulate cholesterol and blood pressure |
| Weight Management | Maintain a healthy weight | Eases strain on the cardiovascular system |
| Foot Care | Inspect feet daily and moisturize properly | Prevents complications |
It’s also critical to manage existing conditions. Keep blood pressure and cholesterol in check, control blood sugar if you have diabetes, and stay up to date with annual flu shots and COVID-19 boosters.
While these steps help lower risk, newer treatments are making a difference in managing PAD.
Latest Treatment Options
Prevention is essential, but advanced treatments are improving outcomes for PAD patients.
For instance, PCSK9 inhibitors like evolocumab have been shown to reduce major cardiovascular events by 27%. Additionally, the VOYAGER PAD trial, involving 6,564 patients undergoing revascularization, revealed that combining low-dose rivaroxaban (2.5 mg twice daily) with aspirin lowers adverse outcomes by 15%.
Key treatment advancements include:
-
Enhanced Lipid Therapy
- Adding ezetimibe to statin therapy
- Using PCSK9 inhibitors for patients not meeting LDL-C goals
- Reducing the risk of major cardiovascular events
-
Advanced Antithrombotic Approaches
- Combining aspirin with low-dose rivaroxaban
- Lowering the likelihood of major limb events in high-risk cases
-
Anti-inflammatory Medications
- Investigating drugs targeting inflammation pathways
- Promising early results in slowing atherosclerosis progression
Additionally, meta-analyses indicate that cilostazol can increase maximum walking distance by 50% and improve pain-free walking distance by 67%. These advances are paving the way for better management of PAD.
Key Takeaways
This section highlights the importance of catching Peripheral Artery Disease (PAD) early and managing it effectively.
PAD impacts about 6.5 million adults in the U.S., often progressing quietly until arterial narrowing becomes severe. Spotting early symptoms is crucial for timely action.
| Key Aspect | Details | What to Do |
|---|---|---|
| Warning Signs | Leg cramps, numbness, slow-healing sores | Keep track of symptoms and inform your provider of any changes. |
| Risk Factors | Age 60+, smoking, high blood pressure | If you’re in a risk group, schedule regular screenings. |
| Treatment Options | Lifestyle changes, medication, surgery | Stick to your treatment plan and follow medical advice. |
Effective management includes making lifestyle adjustments, taking prescribed medications, and working closely with healthcare professionals. Regular exercise and proper medication use can lead to better results, but managing PAD is an ongoing effort that requires attention and care.
FAQs
What are the early signs of Peripheral Artery Disease (PAD) that may require medical attention?
Early signs of Peripheral Artery Disease (PAD) can include cramping, fatigue, or weakness in your legs or arms, especially during physical activity. You might also notice sores or wounds on your legs, feet, or toes that heal slowly or not at all. Other symptoms to watch for include numbness, a feeling of coldness in one limb compared to the other, or changes in the color or texture of your skin.
If you experience any of these symptoms, it’s important to consult a doctor promptly. Early detection and treatment can help prevent the condition from worsening and improve your overall cardiovascular health.
What lifestyle changes can help lower the risk of Peripheral Artery Disease (PAD)?
Making healthy lifestyle changes can significantly reduce the risk of developing Peripheral Artery Disease (PAD) by improving your overall cardiovascular health. Key changes include:
- Quit smoking: Smoking is one of the leading risk factors for PAD, and stopping can greatly improve blood flow and reduce complications.
- Stay active: Regular physical activity, such as walking or light exercise, helps improve circulation and can ease symptoms like leg pain.
- Adopt a heart-healthy diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins while limiting saturated and trans fats to lower cholesterol and prevent plaque buildup in arteries.
These steps not only reduce the risk of PAD but also support better overall heart health. If you’re experiencing symptoms or have concerns, consult a healthcare provider for personalized guidance.
What are the newest treatments for Peripheral Artery Disease (PAD), and how do they help improve patient health?
Recent advancements in Peripheral Artery Disease (PAD) treatment have significantly improved patient outcomes by focusing on both managing symptoms and reducing the risk of serious complications. Key developments include:
- Lifestyle modifications: Quitting smoking, maintaining a heart-healthy diet, and regular exercise are foundational for managing PAD and improving blood flow.
- Medications: High-intensity statins are now standard for lowering cholesterol, while PCSK9 inhibitors offer additional benefits in reducing cardiovascular risks. Blood pressure control (targeting less than 130/80 mm Hg) and antiplatelet therapy have also shown to reduce complications.
- Advanced therapies: Newer medications, such as antithrombotic agents, provide enhanced protection against blood clots, and first-line smoking cessation aids like varenicline improve success rates for quitting.
These treatments, combined with early detection and ongoing care, can help patients manage PAD effectively, reduce symptoms like leg pain and slow wound healing, and lower the risk of serious cardiovascular events.