Heart disease is the leading cause of death in the U.S., but early detection can save lives. Recognizing these seven warning signs can help you take action before it’s too late:
- Chest pain or pressure: A heavy, squeezing sensation that may extend to your arms, neck, jaw, or back.
- Difficulty breathing: Sudden breathlessness, trouble lying flat, or gasping for air.
- Heart rhythm changes: Racing, fluttering, or irregular heartbeats, often paired with dizziness.
- Unexplained fatigue: Persistent tiredness that doesn’t improve with rest.
- Leg and ankle swelling: Fluid buildup causing puffy legs, often worse at the end of the day.
- Sudden sweating with sickness: Cold, clammy sweat paired with nausea or unease.
- Upper body pain: Pressure or tightness in the jaw, neck, arms, shoulders, or back.
Take action immediately if these symptoms occur, especially if they’re severe, persistent, or combined with chest pain or shortness of breath. Early recognition and medical care can make all the difference.
7 Warning Signs of Heart Disease You Should Never Ignore
1. Chest Pain and Pressure
Chest pain or pressure is one of the most common signs of heart disease. Many describe it as a heavy weight pressing on the chest. This feeling might also include squeezing, burning, or tightening and can spread to the arms, neck, jaw, or back [2].
When to Act Quickly: If the pain lasts more than a few minutes or comes and goes, take action within 15 minutes if it doesn’t ease. Suspecting a heart attack? Call 911 immediately [2].
A Note for Women: Women may experience heart attack symptoms differently. While chest pain is still frequent, they might also feel discomfort in areas like the jaw, neck, shoulders, or upper stomach [3].
Heartburn or Something More? Heartburn can sometimes feel similar to a heart attack. However, if the pain is severe, persistent, or accompanied by shortness of breath or dizziness, treat it as a medical emergency [2][3].
Chest pain is often the first clue that something might be wrong with your heart. Recognizing it early can make all the difference. Next, we’ll look at another key sign: difficulty breathing.
2. Difficulty Breathing
Shortness of breath is a major warning sign of heart problems that needs immediate attention. While chest pain is widely recognized, struggling to breathe can also indicate heart trouble. The American Heart Association reports that this symptom is experienced by about 42% of women and 30% of men during heart attacks [5].
When the heart isn’t pumping effectively, fluid may build up in the lungs, making breathing difficult. This can point to conditions like heart failure or coronary artery disease [2][4]. The symptom might come on gradually or strike suddenly, happening during physical activity or even while resting.
Signs You Shouldn’t Ignore
- Sudden breathlessness without an obvious reason
- Trouble breathing when lying flat
- Waking up gasping for air
- Feeling out of breath during everyday activities
When to Get Emergency Help
If shortness of breath is paired with other heart attack symptoms – like chest discomfort or dizziness – seek emergency medical care right away [2][3]. People with conditions such as high blood pressure or diabetes should be especially cautious.
Other Emergency Symptoms to Watch For:
Spotting these signs early is critical, especially since heart failure impacts over 6.2 million adults in the U.S. [5]. Up next, we’ll look at how changes in heart rhythm can reveal hidden heart issues.
3. Heart Rhythm Changes
Irregular heartbeats, known as arrhythmias, impact millions of Americans. Atrial fibrillation is one of the most frequent heart rhythm disorders [5].
Common Warning Signs
Be alert to these symptoms that might indicate a heart rhythm issue:
- A racing, fluttering, or skipping heartbeat
- Noticeably fast or slow pulse
- Feeling dizzy or lightheaded, especially when standing [1][3]
Types of Heart Rhythm Problems
| Type | Description | Key Symptoms |
|---|---|---|
| Atrial Fibrillation | Irregular beats in the upper chambers | Fluttering, fatigue |
| Fast Heartbeat | Abnormally rapid heart rate | Racing heart, breathlessness |
| Slow Heartbeat | Unusually slow heart rate | Weakness, dizziness |
Risk Factors
Certain conditions or traits can raise the likelihood of arrhythmias [4][7]:
- Heart-related problems (e.g., high blood pressure)
- Diabetes
- Getting older (risk increases after 45 for men, 55 for women)
When to Seek Emergency Care
Contact emergency services immediately if you experience:
- Chest pain combined with an irregular heartbeat and trouble breathing
- Fainting or near-fainting
- Persistent or frequent dizziness lasting several minutes [1][3]
Sometimes, arrhythmias occur without clear symptoms [6]. Factors like too much caffeine or stress can also bring them on [8]. Adopting a heart-healthy lifestyle can help reduce these triggers.
Catching arrhythmias early is crucial to avoid complications like stroke or heart failure. Even subtle signs, such as unexplained fatigue, can point to underlying heart rhythm issues. Keep an eye out for these warning signals.
4. Unexplained Tiredness
Feeling constantly tired might seem normal in today’s busy world, but it could be an early warning sign of heart disease, especially when paired with other symptoms. The American Heart Association notes that up to 70% of people with heart failure report experiencing significant fatigue [7].
Why Heart Issues Lead to Fatigue
When the heart isn’t pumping efficiently, tissues don’t get enough oxygen, making the body work harder to compensate. This reduced blood flow also causes waste products to build up, which contributes to the feeling of exhaustion [4][9].
How to Spot Heart-Related Fatigue
Heart-related fatigue stands out because it doesn’t improve with rest, shows up even after light activity, and can linger for weeks or even months.
Fatigue and Gender Differences
Women, in particular, should be cautious. Studies reveal that 70% of women who had heart attacks reported fatigue as one of their main symptoms [5].
When to See a Doctor
If fatigue is disrupting your daily life, or if it’s paired with symptoms like shortness of breath, chest discomfort, or an irregular heartbeat, it’s time to consult a doctor [4][9].
Persistent tiredness might not always mean heart disease, but it’s a clue you shouldn’t ignore – especially if it comes with other signs mentioned earlier. Next, we’ll look at how swelling in the legs and ankles can also hint at heart problems, another symptom that often goes unnoticed.
sbb-itb-4bfbcfd
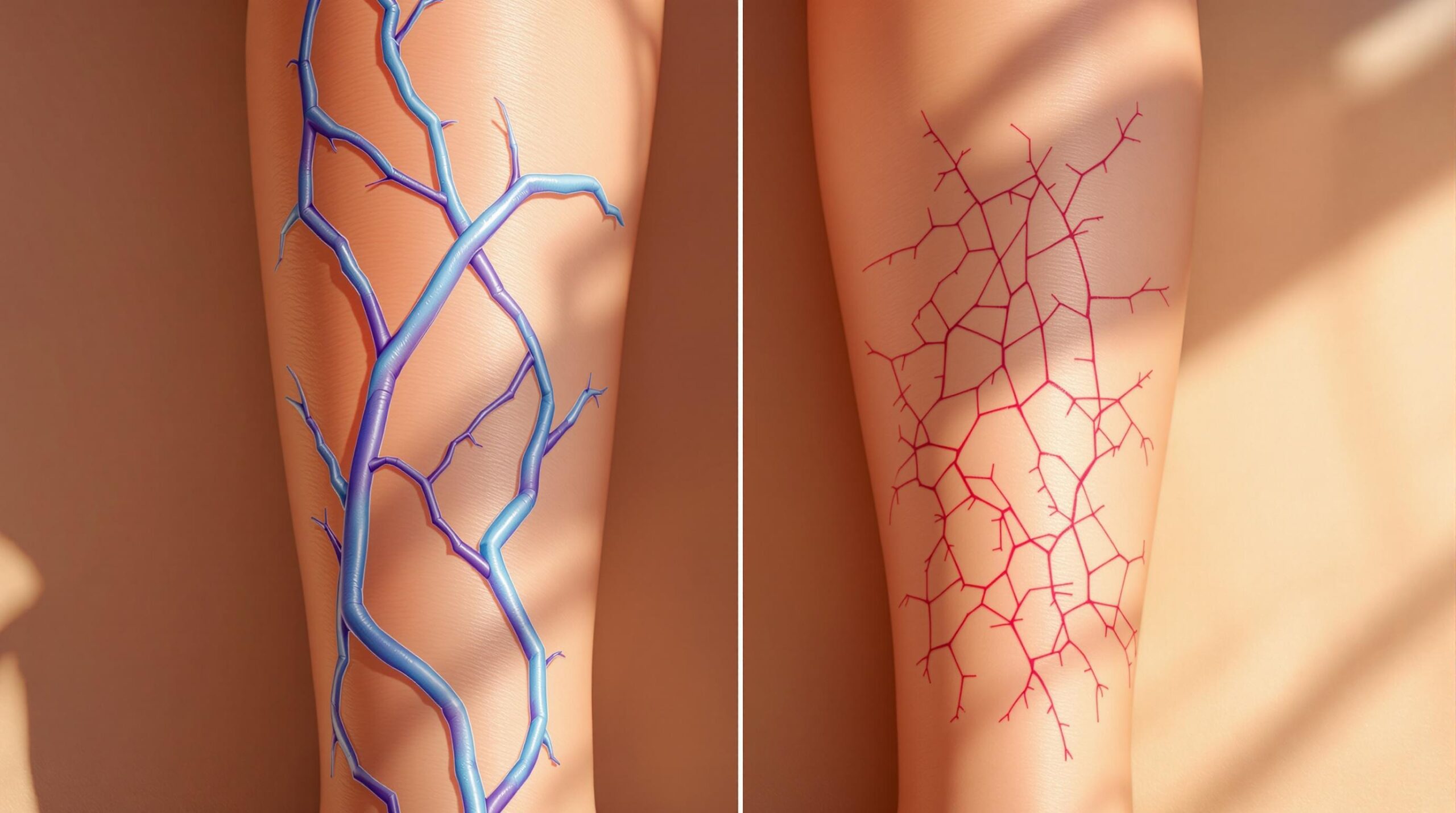
5. Leg and Ankle Swelling
Swelling in the legs and ankles can be a warning sign of heart problems. When the heart isn’t pumping efficiently, blood flow decreases, leading to fluid buildup. This fluid often collects in the legs and ankles due to gravity [4].
The American Heart Association reports that this symptom is common among the 6.2 million adults in the U.S. living with heart failure. Swelling tends to worsen as the day goes on but may ease slightly after a night’s rest.
What to Look For
Swelling caused by heart issues often appears in both legs equally. It can get worse after sitting or standing for long periods, improve when you elevate your legs, and may leave an indentation when pressed (known as pitting edema) [4].
When to Seek Help
Prime Heart and Vascular stresses that sudden or severe swelling – especially if paired with shortness of breath or chest pain – requires immediate medical attention. Even gradual swelling should be checked by a healthcare professional to identify the cause.
Tips for Temporary Relief
If you’re dealing with swelling, you can try a few simple steps to ease it:
- Elevate your legs above heart level
- Cut back on salt in your diet
- Stay active
- Avoid sitting or standing for long stretches
Swelling is just one potential sign of heart trouble. Up next, we’ll discuss how sudden sweating combined with feeling unwell can also point to heart issues.
6. Sudden Sweating with Sickness
Sudden sweating paired with nausea can be an alarming sign of heart disease, especially during a heart attack. Many people mistake these symptoms for the flu or anxiety, but understanding their importance could make all the difference.
"If you’re experiencing nausea or profuse sudden sweating accompanied by other symptoms such as chest discomfort, shortness of breath and pain in the upper body, it may be a sign of a heart attack." – Dr. Gary J. Rogal, Medical Director for Cardiovascular Services at RWJBarnabas Health [10]
Recognizing the Signs
Unexplained, sudden sweating – particularly when it feels cold or clammy – may indicate the heart isn’t getting enough oxygen. This can happen without warning, regardless of your activity level or the surrounding temperature. Often, it’s accompanied by nausea or a general feeling of unease.
Here’s what to watch for:
- Sudden, heavy sweating not linked to heat or physical activity
- Sweat that feels cold or clammy
- Nausea or an overall feeling of sickness
Women and Heart Attack Symptoms
Women often experience heart attacks differently than men. Symptoms like sweating and nausea can appear without the typical chest pain, making it even more important to recognize these less obvious signs [3].
What to Do in an Emergency
If sweating and nausea occur alongside chest discomfort, upper body pain, or shortness of breath, it’s time to act. The American Heart Association stresses that quick recognition and immediate medical attention are critical [5].
Staying Ahead of the Risk
Regular health check-ups and maintaining a heart-friendly lifestyle can lower your risk. Acting quickly when symptoms arise can greatly improve your chances of avoiding severe complications.
Sweating and nausea often appear with other symptoms, like upper body pain, which will be covered next.
7. Upper Body Pain
Heart disease pain isn’t always confined to the chest – it can show up in unexpected areas of your upper body.
Where Pain Can Show Up
Heart-related pain in the upper body often feels like pressure, tightness, or a squeezing sensation. Common areas include:
- Jaw and neck
- Either arm (not just the left)
- Shoulders
- Upper back
Differences Between Men and Women
Women might feel heart-related pain in the jaw, neck, or arms, sometimes without any chest discomfort. This can delay treatment, as these symptoms are often overlooked or misinterpreted [3][4]. Understanding these variations is key to acting quickly.
When You Should Act
Seek medical help immediately if upper body pain:
- Lasts for several minutes or more
- Comes and goes in waves
- Happens with other symptoms like shortness of breath
- Gets worse with physical activity
How to Spot the Difference
| Heart-Related Pain | Less Concerning Pain |
|---|---|
| Starts suddenly | Develops gradually |
| Spreads to multiple areas | Stays in one spot |
| Comes with other symptoms | No other symptoms |
| Doesn’t improve with rest | Eases with rest |
| Feels like pressure or squeezing | Feels sharp or stabbing |
What to Do in an Emergency
If you have unexplained upper body pain, especially with other symptoms, don’t try to self-diagnose. According to the American Heart Association, calling emergency services is critical – don’t drive yourself to the hospital [2][3].
Recognizing these signs can save lives, but acting on them immediately is just as crucial.
Next Steps and Medical Care
When to Call Emergency Services
Severe heart disease symptoms, like chest pain lasting more than a few minutes, require immediate medical attention [5].
In such cases, call 911 right away. While waiting for help, chew a 300mg aspirin (if you’re not allergic) and try to stay calm and still [6][5]. Having a plan in place for emergencies can make all the difference.
Urgent vs. Non-Urgent Symptoms
| Symptom Type | Action Required | Timeframe |
|---|---|---|
| Severe chest pain | Call emergency services | Immediate |
| Stable angina | Contact doctor | Within 24 hours |
| New/changing symptoms | Schedule appointment | Within a week |
Stable angina often improves with rest. However, if symptoms persist for more than 15 minutes, it could signal a heart attack and demands immediate action [6].
Staying proactive about your heart health can help you avoid emergencies.
Regular Heart Health Monitoring
Routine check-ups are essential, especially if you have a family history of heart disease or other risk factors [4]. During these visits, make sure to discuss:
- Any new or ongoing symptoms
- How well your medications are working
- Adjustments to your lifestyle
- Ways to manage risk factors
Preparing for Medical Visits
Make the most of your doctor appointments by coming prepared. Keep a record of your symptoms, update your medication list, note any lifestyle changes, and share any relevant family history.
Managing Chronic Heart Conditions
If you have a chronic heart condition, understanding the difference between stable and emergency situations is key. Stable angina usually improves with rest or medication within 10 minutes. But if symptoms last longer than 15 minutes, it could indicate a heart attack and requires immediate help [6].
Keep in mind that some heart attacks can occur without obvious symptoms, particularly in older adults or individuals with diabetes [6]. Regular monitoring and awareness can help you stay ahead of potential complications.
FAQs
How long should chest pain last before going to the doctor?
If chest pain lasts more than 5 minutes and doesn’t improve with rest or medication, it’s time to get emergency help right away [1]. This is especially urgent if the pain feels:
- Severe or crushing
- Paired with shortness of breath
- Radiating to your arms, neck, or jaw
The American Heart Association warns that delaying care can be dangerous [4]. Here’s what to do if you’re experiencing chest pain:
- Call 911 immediately and try to stay calm.
- If advised and not allergic, take 300mg of aspirin.
- Note when the symptoms started and their severity while waiting for help.
Chest pain lasting over 15 minutes could signal a heart attack [6]. For individuals with diabetes, symptoms may be harder to notice, so even mild discomfort should be taken seriously [6].
It’s also worth noting that women may experience different warning signs than men. Instead of classic chest pain, they might feel upper body discomfort, nausea, or other symptoms [3]. Acting promptly can make a critical difference.