Varicose veins and spider veins are often confused, but they differ in appearance, causes, and risks. Varicose veins are large, bulging veins (3-8mm thick) that develop deeper in the legs, often causing pain and health risks like ulcers or blood clots. Spider veins are thin, web-like veins (<1mm thick) near the skin’s surface, usually found on the legs or face, and are mostly cosmetic.
Key Differences at a Glance:
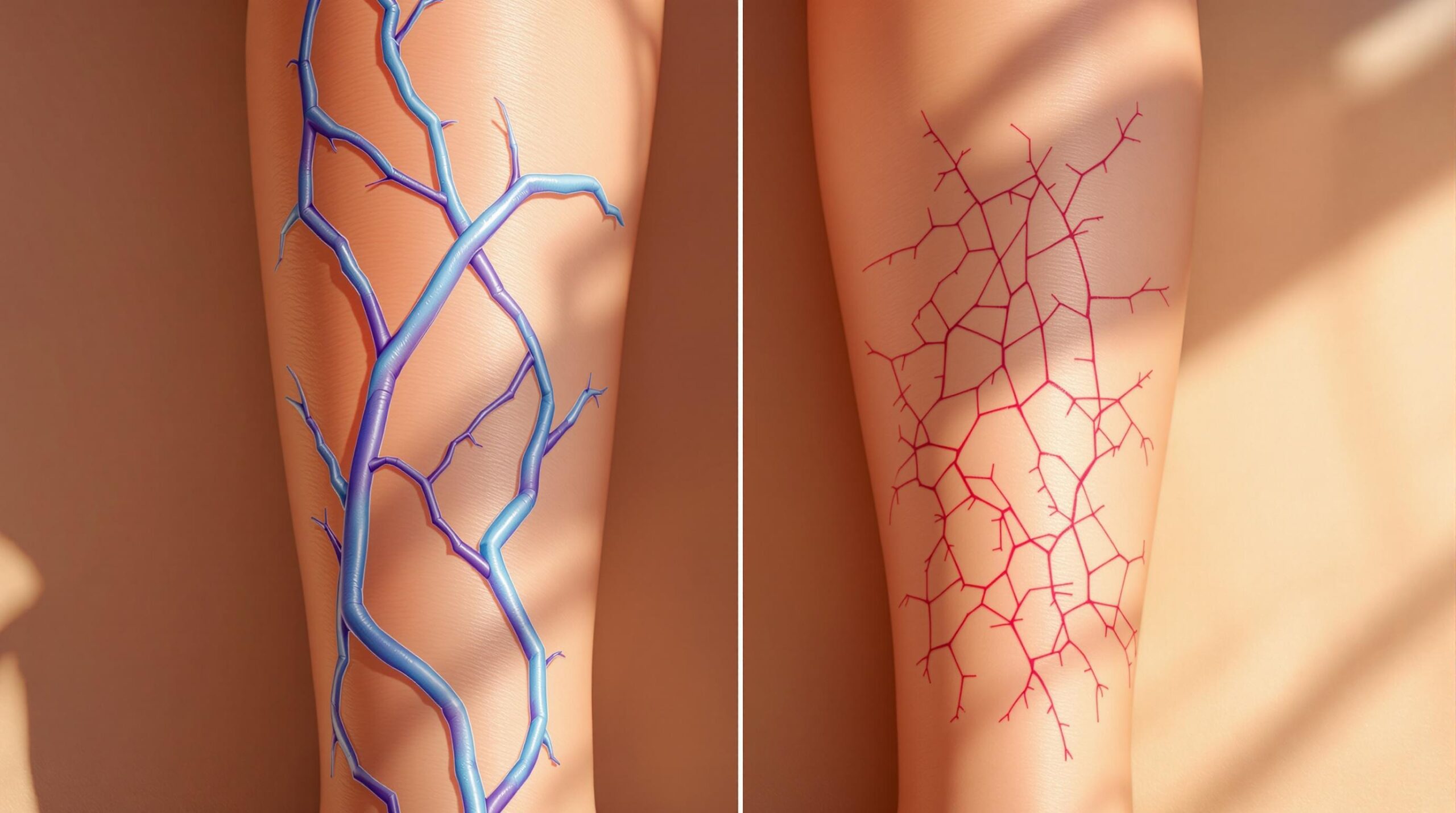
- Varicose Veins: Bulging, rope-like, dark purple/blue, deeper veins, often painful, linked to circulatory issues.
- Spider Veins: Thin, flat, red/blue patterns, closer to the skin, usually painless, cosmetic concerns.
Quick Comparison Table:
| Feature | Varicose Veins | Spider Veins |
|---|---|---|
| Size | 3-8mm thick, bulging | <1mm thick, flat |
| Location | Legs, feet | Legs, face |
| Color | Dark purple/blue | Red, blue, or purple |
| Depth | 1-3mm below skin | <0.5mm below skin |
| Symptoms | Pain, heaviness, swelling | Mild burning, itching |
| Health Risks | Ulcers, blood clots, skin damage | Rarely causes health issues |
| Treatment | Medical (e.g., EVTA, surgery) | Cosmetic (e.g., lasers, sclerotherapy) |
Takeaway: Varicose veins often require medical attention due to health risks, while spider veins are typically treated for cosmetic reasons. Both conditions benefit from early diagnosis and proper care.
Spider Veins vs Varicose Veins: Understanding Key Differences
Physical Differences: How They Look and Where They Appear
These conditions show clear visual markers that play a major role in accurate diagnosis. These details are essential for understanding the diagnostic methods discussed later.
Size, Color, and Location Comparison
Varicose veins appear as rope-like, bulging veins in the legs, while spider veins form flat, web-like patterns on the legs or face. Their colors also differ: varicose veins are typically dark purple or blue, though visibility can vary depending on skin tone. Spider veins, on the other hand, display a wider range of colors:
| Vein Type | Color | Location | Origin |
|---|---|---|---|
| Arterial Spider Veins | Bright Red | Face, Upper Body | Capillary Dilation |
| Venous Spider Veins | Blue/Purple | Legs, Lower Body | Venous Blood Pooling |
Another key difference lies in how deep they are beneath the skin. Varicose veins develop deeper, typically 1-3mm below the surface, causing the shadowy, raised bulges you can see and feel. Spider veins, by contrast, form in the topmost skin layer (less than 0.5mm deep), creating fine, flat patterns. While varicose veins feel raised to the touch, spider veins remain smooth.
A common spider vein pattern is the "corona phlebectatica" – fan-shaped veins radiating around the ankles. This pattern is often linked to venous insufficiency risks, which are covered in the Health Risks section. These visual differences also tie into their varying risk factors, which are discussed next.
Causes and Risk Factors
Varicose veins and spider veins both result from problems with vein valves, but the underlying issues differ. Varicose veins are linked to deeper vein system failures, while spider veins usually involve fragile surface vessels. The difference in vein size and depth explains their distinct appearances.
Common Risk Factors
Both conditions are caused by venous insufficiency, where weakened valves allow blood to flow backward. Whether varicose veins or spider veins form depends on the size and depth of the affected veins.
Specific Causes for Each Type
Varicose Veins are primarily caused by structural problems in the veins. Genetics play a major role – if both parents have varicose veins, there’s a 90% chance of inheriting the condition. Chronic venous insufficiency is another key factor in their development.
Spider Veins have their own specific triggers:
- UV exposure can weaken the walls of surface veins.
- Hormonal changes, such as those during pregnancy, may contribute.
- They often form without any deeper venous issues [7].
Recent studies highlight enzymes that degrade vein wall proteins as contributors to these conditions. These biological differences explain why varicose veins are often linked to circulatory strain, while spider veins tend to result from surface-level factors. This distinction also ties into their cosmetic differences, as noted in Physical Differences.
Signs and Health Risks
Varicose Veins: Warning Signs and Complications
Varicose veins aren’t just a cosmetic issue – they often come with physical discomfort and potential health problems. Common symptoms include leg heaviness and nighttime cramps. These symptoms tend to get worse after standing for more than 30 minutes.
Chronic blood pooling increases venous pressure (by 10-12 mmHg), which can lead to a range of complications. Here’s a breakdown of some of the more severe cases:
| Complication | Risk Rate | Impact |
|---|---|---|
| Venous Stasis Ulcers | 40% recurrence within 5 years | Chronic wounds that heal slowly |
| Superficial Thrombophlebitis | 4-62% lifetime risk | Blood clots and inflammation |
| Chronic Venous Insufficiency | 30-40% progression rate | Poor circulation and tissue damage |
"Untreated cases risk restricting circulation to the skin through progressive fluid leakage", says Dr. Palma M. Shaw.
Spider Veins: Effects and Concerns
Spider veins are generally less risky than varicose veins, but they can still cause issues. While often seen as a cosmetic problem, they may lead to:
- Localized itching or burning, which can be uncomfortable.
- Mild skin irritation, affecting daily comfort.
While spider veins might seem harmless, they shouldn’t always be ignored. According to the Upstate Vascular Institute, professional evaluation is key, especially when they signal circulation problems or cause ongoing discomfort.
Understanding these distinctions helps guide the right approach to treatment, which we discuss in the next section on Treatment Methods.
sbb-itb-4bfbcfd
Medical Tests and Diagnosis
Identifying medical conditions depends on understanding visual differences and risk patterns, as previously discussed.
Testing for Varicose Veins
Diagnosing varicose veins involves advanced imaging techniques to evaluate blood flow and valve performance. The go-to method is duplex ultrasound, which merges two imaging technologies to create detailed vein maps.
Specialists typically perform three main assessments during the examination:
| Test | Purpose |
|---|---|
| Standing Scan | Evaluates pressure changes |
| Valsalva Maneuver | Identifies valve leaks at critical leg vein junctions |
| Calf Movement Test | Measures blood-pumping efficiency |
The ultrasound focuses on signs of venous insufficiency. One key indicator is reflux lasting more than 0.5 seconds during calf compression and release. These tests help detect changes in venous pressure, as noted in the Health Risks section.
"Venous mapping via ultrasound guides treatment planning for symptomatic cases"
Checking for Spider Veins
Spider veins are usually diagnosed through visual examination because they are close to the skin’s surface. During a physical exam, doctors look for specific traits:
| Visual Indicator | Importance |
|---|---|
| Skin Condition | Confirms no ulceration or tissue changes |
Although advanced imaging isn’t typically needed for spider veins, additional tests may be required in certain situations. These include:
- Unexplained rapid spread
- Swelling or heaviness similar to varicose vein symptoms
- Family history of deep vein thrombosis
Vascular specialists often use the CEAP classification system (Clinical-Etiological-Anatomical-Pathophysiological) to organize their findings. This approach links cosmetic patterns to potential underlying venous issues, aiding both diagnosis and treatment planning while distinguishing between cosmetic and medical concerns.
Treatment Methods
After diagnosis through techniques like duplex ultrasound and visual exams, treatment plans are tailored based on the severity of the condition. Varicose veins often require more intensive medical procedures, while spider veins are usually addressed with less invasive methods.
Comparing Treatment Options
The choice of treatment largely depends on how severe the condition is and its underlying causes. For varicose veins, treatments often focus on medical necessity, whereas spider vein procedures are typically cosmetic.
| Treatment Type | Varicose Veins | Spider Veins |
|---|---|---|
| Duration | 45-90 minutes | 15-30 minutes |
| Recovery Period | 1-7 days | 0-2 days |
| Results Visible | 2-6 weeks | 3-8 weeks |
Modern Treatment Options
Recent advancements have made vein treatments more effective and less disruptive to daily life. For example, Endovenous Thermal Ablation (EVTA) boasts a 94% success rate for varicose veins. This is particularly important since varicose veins have a 30-40% chance of progressing to chronic venous insufficiency. EVTA is a quick procedure, typically under an hour, with most patients resuming normal activities within 1-2 days.
For spider veins, cutting-edge technologies include:
- Specialized lasers targeting shallow veins at a depth of 0.5mm
- Combination therapies using sclerosing agents and laser treatments
- Precision micro-incision techniques for improved accuracy
Advanced laser systems clear 80-90% of spider veins. Combining therapies can improve results by 15-20% compared to single-method treatments. Post-treatment care differs depending on the condition:
| Post-Treatment Care | Varicose Veins | Spider Veins |
|---|---|---|
| Recovery Guidelines | 2-6 weeks compression, avoid heavy lifting for 1 week | 1-3 weeks compression, no major restrictions |
| Follow-up Needs | Ultrasound at 6 weeks | Visual check |
These treatment outcomes play a key role in shaping prevention strategies, which are discussed in the next section.
Prevention Steps
Effective prevention strategies address the specific causes discussed earlier:
Basic Prevention Methods
Incorporating movement and making small lifestyle changes can make a big difference, especially when done consistently. Here’s a simple plan:
| Activity Type | Duration | Frequency | Benefits |
|---|---|---|---|
| Walking | 30 mins | Daily | Improves circulation |
| Leg elevation | 15-20 mins | 2-3x daily | Reduces pressure |
| Calf raises | 15 reps | 2x daily | Strengthens muscles |
Keeping a healthy weight can lower leg vein pressure by 40–50%. For those who stand for long periods, anti-fatigue mats help reduce venous pressure by 18%. If you work at a desk, taking a 5-minute walking break every hour and ensuring proper ergonomic setup can significantly lower risks.
While these general tips apply to both conditions, there are also specific strategies based on individual risk factors.
Targeted Prevention Tips
For Varicose Veins: Sleeping on your left side during pregnancy can ease pressure on the vena cava, a major vein.
For Spider Veins: Regular use of SPF can protect against facial vein patterns like arterial spider veins. Be mindful of hormonal factors – birth control pills can raise the risk of spider veins by 70% in individuals with a predisposition.
Screening recommendations depend on personal and professional risk factors:
- Family history: Consider an ultrasound at age 35.
- High-risk jobs: Vein mapping is recommended by age 35.
- Pregnancy: Monitoring during the first trimester is helpful.
For professions with higher risks, like teaching or factory work, workplace adjustments are crucial. For instance, ergonomic setups in factories have been shown to reduce vein-related issues by 40% [7]. Compression garments are especially beneficial for teachers and nurses during long shifts.
"Prophylactic measures, when started early, can prevent up to 58% of pregnancy-related varicose veins. The key is using appropriate compression garments (20-30 mmHg) from the first trimester."
Conclusion
Understanding the differences between varicose veins and spider veins is crucial for making informed care decisions. Varicose veins often point to issues with the circulatory system, while spider veins are generally a cosmetic concern unless they cause discomfort.
The level of medical attention needed depends on the symptoms and how the condition presents. Here’s a quick reference for common symptoms and recommended actions:
| Key Symptoms | Action Needed |
|---|---|
| Leg swelling with skin changes | Seek immediate medical attention |
| Sudden vein inflammation | Requires emergency evaluation |
| Spider veins with leg heaviness | Schedule a medical check-up |
Treatment options can address both health risks and cosmetic concerns. As discussed earlier, successful management involves tailoring diagnostic and treatment strategies to fit each patient’s unique needs and circumstances.